Therapeutic Ketosis: Let’s Get Real!
If you’re about to adopt a ketogenic diet for cancer, there’s a good chance you’ve come across the Glucose Ketone Index. This can be an tough topic so let’s start with a summary to lay the groundwork.
GKI (Glucose Ketone Index) is a ratio of blood glucose to ketones.
Therapeutic ketosis for cancer patients is defined as a GKI of 1-2, but this range was derived from studies on mice and may not be appropriate for all human patients.
Factors like stress, medication, and age can affect a person's ability to achieve and maintain a GKI in the therapeutic range.
A GKI of 5 can still be beneficial, and any effort to limit glucose spikes can help weaken cancer cells.
Fasting and modified fasting can be effective strategies for achieving therapeutic ketosis, but should be done with caution, especially for those who are already weakened.
It is important to consider individual factors such as age, weight, and overall health when determining whether a long fast or rigorous keto diet is appropriate.
Be cautious of online information about cancer cures, and consult with a healthcare professional before making any major changes to your diet or treatment plan.
Glucose Ketone Index (GKI).
The term GKI was coined by Dr. Thomas Seyfried, a cancer researcher at Boston College, to describe the ratio of blood levels of glucose to ketones when both are expressed in mmol/L units (18 mg/dL equals 1 mmol/L). Click here for the paper.
Therapeutic ketosis is defined as a GKI of 1-2: Notably, Seyfried’s mice had glucose levels that were generally in the range of 3 mmol/L (~55-65 mg/dL) with ketone levels above 3 mmol/L.
How do you calculate the GKI?
Easy! Divide the ketone reading by the glucose reading.
A few simple examples:
A reading of 3 mmol/L glucose and 3 mmol/L ketones represents a GKI of 1
A reading of 4 mmol/L glucose and 2 mmol/L ketones represents a GKI of 2
So here’s the backstory: GKI and therapeutic zone numbers for cancer came from Dr. Seyfried’s mouse model research on young mice, in the prime of life, with robust and intact immune systems, who were newly implanted with cancer cells that predictably proliferated and metastasized. Importantly (but rarely considered), these mice were not stressing over their cancer diagnosis or worried about family, work or finances. Their food was provided to them on schedule and their cages kept clean. The mice that responded best (GKI of 1-2) were losing fat and muscle (“catabolic”) throughout the study period. This metabolic stress, more typical of starvation rather than a “fed state,” helped to limit cancer progression. For these mice, the benefit most likely outweighed the muscle loss but let’s be real: no one was concerned with whether or not the mice would regain lost weight or recover muscle mass. And notably, none of them became cancer free. (Sorry, mice…)
Now compare the mouse model to a typical human with a cancer diagnosis whose world has been turned upside down: stressors are off the charts, and the disease and treatments are taking their toll on mental, physical, and financial health. Appetite may be poor and sleep is in shambles. Medications, typically steroids, prescribed to lower the inevitable inflammation raise glucose and depress the immune system. Is this a good time to strive for that Holy Grail of a GKI of less than 2? Absolutely not!
If what I just described is similar to the situation you find yourself in right now,consider this: You might get to that optimal GKI during a long water-only fast, or if you are “calorically restricted, limiting fat as well as carbs). Both of these strategies will push your body into breaking down more fat, an effective (and perhaps desirable) short-term strategy during the first few weeks or months but it is not sustainable over time, especially if you are older or already at a low weight.
Should you abandon keto if you can’t reach that ideal GKI? Not so fast.. Dr. Dom D’Agostino and I agree that a GKI of 5 is still enviable AND therapeutic! And any effort to limit spikes in glucose (which in turn lowers insulin secretion) may aid in weakening cancer cells. That can usually be achieved with some combo of carb restriction, protein management, sufficient fat intake and ketone supplementation. Lifestyle improvements (maintaining fitness; lowering stress; improving sleep) also contribute to better glucose control. Keeping to an 8-10 hr eating window and engaging in “modified fasting” around your infusion treatments add to the metabolic pressure on cancer cells.
Is there ever a good time to up your game on reaching therapeutic ketosis?
Let me introduce some personal bias here: At Dietary Therapies, we believe strongly that the majority of people will experience fewer or less severe GI side effects if they fast - strategically - on either side of their infusion treatments. They may also see more a more profound impact on their cancer (based mostly on their expected response to treatment). So far, the evidence for a benefit has been limited to conventional treatment scenarios but people are already using this “off-label” fasting strategy with alternative treatments as well, pushing to get into therapeutic ketosis in the days surrounding treatments and returning to a more moderate plan outside of that window. In any case, lowering inflammation associated with treatment is always a good thing in cancer!
There is also a growing interest in using this type of short-term intervention to restrict glutamine and methionine; amino acids that are essential to life but have been hijacked by many (if not most) types of cancers to fuel progression. Conventional cancer research is looking into developing cash-cow pharmaceuticals but if you are reading this today, my guess is that you don’t have the luxury of time on your side for drug approvals. If you do opt for dietary restriction of these amino acids through fasting, be careful. For those who are already weakened by the impact of their disease or by continuous cycles of treatment, the plan should be modified to reduce the potential for harm. Consider working with our team if you need this kind of support.
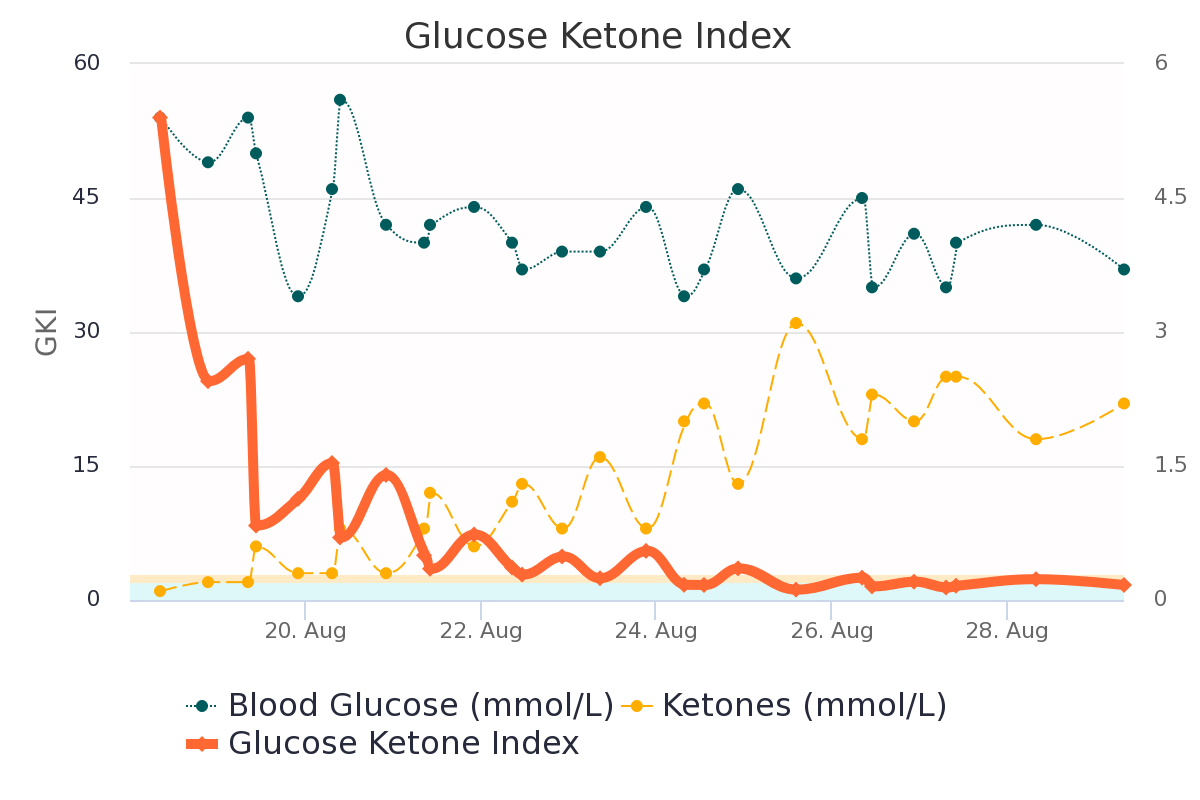
A real-world look at therapeutic ketosis, with the help of a client’s chart:
Used with permission
I pulled this chart from a client’s Cronometer, my preferred tracking tool. This shows the change in GKI as my client began to implement the plan we worked out together. The solid orange line represents the GKI index: it fell from a high of around 53 to below 3 (yay!) over the course of just one week! The green dotted line is glucose; the Y axis shows readings in mmol/L. Glucose was fairly normal to start but look what happened to ketones, represented by light orange dots: It rose from a low of around 0.5 mmol/L on the first day to a high of 3 mmol on Aug 25th.
Next up, a 3-month GKI chart from another client:
Used with permission
The dark orange line in the blue zone at the bottom of the chart represents that optimal GKI of 1-2. The peach zone is a GKI of 2-3: Also therapeutic! These ranges are usually obtainable in people who can maintain a rigorous keto diet: keeping carbs very low, managing protein intake to maintain muscle, and filling in with enough fat to sustain high ketosis, maybe even adding in a ketone supplement. Young children usually stay in this zone easily given their relatively low protein needs but it does become more of a challenge for teens in growth spurts. Adults in their 20’s and even into their 30’s may also keep in this zone, especially if they are metabolically healthy despite their cancer diagnosis. But with each successive decade, changes in our overall metabolic health start working against us.
The impact on GKI from the disease and its treatment is clearly seen in this final chart!
Used with permission
This chart is from from a young man in his 20’s with a brain tumor who was hospitalized and treated with high-dose steroids following an extreme reaction to his first infusion of a trial drug. Look at what happened to his GKI! Notably though, his glucose didn’t go sky high as you might expect, probably due to his young age and insulin sensitivity. But look what happened to his ketones: they dropped off the cliff because the action of steroids suppressing ketosis through several pathways. As blood counts recovered, he was weaned from the steroid medication. The step-down that you see at the end of the first week in July matched the step-down in dosage but the effect on GKI lingered for another couple of weeks.
I wish I had a bit-coin for every time that a client reaches out in panic when they see this happen to their numbers. A common reaction: “I failed, so I need to tighten up even more on my diet!” My usual reply: “Steroids are in the driver’s seat right now, jacking up glucose and creating insulin resistance which makes it so much harder for your large muscles to clear excess glucose. Tightening up may help minimally in the short term but stressing over an ideal GKI will work against you over time. More restriction will break down your body’s already stressed reserves of muscle and fat. That will definitely have a net negative effect on your quality of life!” If treatments and/or disease progression are keeping inflammation high, I go on to warn them that this perfect storm may fuel cachexia, that deadly catabolic cascade responsible for “poor outcomes” in many cancers. I can usually see that unfolding in some of their blood biomarkers. My advice here is to prioritize a higher intake of protein and fat, using veggies and berries as “condiments” to increase palatability. And take some ketone supplements for their anti-inflammatory potential, sparing muscle even if you can’t’ maintain ketosis in the therapeutic zone.
Please understand that I’m not trying to crush your hope for a cure. I’m just trying to keep you safe from all the confusing information, well-meaning misinformation, and deliberate disinformation that we are all exposed to now in our digital lives.
Here’s what I see happening: You read a post or watch a video claiming that cancer disappeared with fasting. And that triggers an algorithm that feeds you the next post or video. And the next... But the realty is that there are only a limited number of cases with enough evidence to suggest that the cancer did in fact result in “no evidence of disease;” referred to as “radical remission” in the alternative space. But let’s be clear: many of these early successed do see a recurrence weeks or months down the road but fail to update their online story. And most of the durable successes are limited to “treatment naive” individuals who might undergone surgery that removed the bulk of the cancer before they were worn down by disease progression or multiple rounds of treatment.
My outrage is reserved for scammers and influencers in both the conventional and alternative spaces who promote half-truths and outright lies to prey on people’s fears and vulnerability, using their elevated online status to line their own pockets.
Unfortunately, I have yet to see anyone with aggressive late-stage disease, already malnourished and immune-compromised, with tumor load keeping inflammation and glucose high, succeed at using a long fast or rigorous keto diet to pull out of a catastrophic downward spiral. You owe it to yourself (or your loved one) to examine all the variables seen with fasting (and other “I cured my cancer” stories). There is a tipping point where age, weight, liver and kidney function, immune system status, mobility impairment and other health factors should lead you to question if you (or your loved one) will be helped or harmed by engaging in a long fast.